What Is Restrictive Practice?
In health and social care, restrictive practices are sometimes used to keep people safe when there’s a serious risk of harm to themselves or others. These practices involve limiting a person’s freedom of movement or their human rights in very specific situations. They can take different forms, such as physical restraint, chemical restraint, environmental restraint, or seclusion.
However, restrictive practices should never be the first response. They’re meant to be a last resort, used only in extreme circumstances when all other approaches have been tried and haven’t worked. The focus is always on safety, dignity, and respect.
There are strict legal and ethical safeguards in place to make sure these interventions are used appropriately. This includes getting consent where possible, using the least restrictive option, keeping the intervention as short as possible, and reviewing it regularly. Above all, every decision should reflect a person-centred approach, recognising the person’s rights, preferences, and wellbeing.
When used in the right way, with careful thought and oversight, restrictive practices can help prevent harm while still upholding the values of compassionate and respectful care.
Can Restrictive Interventions Be Harmful?
Yes. Restrictive interventions can have serious and lasting consequences. They may result in physical injuries, such as fractures or soft tissue damage, and cause psychological harm, including post-traumatic stress (PTSD) and re-traumatisation. Beyond the physical and emotional impact, these interventions can take away a person’s dignity, human rights, and sense of autonomy.
Some high-risk methods, such as prone restraint, carry life-threatening dangers, including asphyxiation. This is why the focus across health and social care is on eliminating restrictive practices and creating a culture that protects dignity, promotes well-being, and upholds people’s rights at every stage.
Restrictive practices have the base principles in limiting one’s freedom and ability to engage in day-to-day activities. Also, they are known to reduce meaningful interactions with family, support staff and carers.
The prolonged use of a restrictive practice may ultimately lead to over-reliance, which means people lose their ability to live independent and active life. That’s why it is essential to always focus on the people’s unique needs, skills, and abilities and have a positive approach so people can feel safe and secure.

Positive Approaches to Reduce Restrictive Practices in Health and Social Care
Positive approaches are based on using proactive strategies which prioritise positive reinforcement and strengths-based methods.
Through the positive approach, family, friends, and carers can learn what their loved ones like or dislike, what kind of skills and abilities they have, and how to respect and value their backgrounds. Also, they can learn how to communicate and understand the environment’s impact on their loved ones by consistently looking for other ways of support in every aspect of care.
A positive approach focuses on working closely with people and their support networks to truly understand how they are feeling and what changes might help in their daily lives. This involves identifying what needs to be adapted, planned, or structured so the person can feel calm, supported, and in control, which minimises the risk of the need of using restrictive interventions.
Positive Behaviour Support (PBS)
Positive behaviour Support (PBS) has been developing for the past 30 years. It is an evidence-based approach built on positive reinforcement, where attention is directed towards meaningful and purposeful activities. PBS starts by truly understanding the person – what motivates them, what they’re good at, and what makes life harder for them.
The main focus of PBS is to improve quality of life by learning all the reasons why and how people use their behaviour to communicate and meet their needs. By learning, we can all start understanding how to build better support, work towards positive outcomes and improve the services that people receive.
The positive behaviour support plan is always created with the person being supported and their family and carers. A PBS plan will be built upon person-centred strategies and will assist in building alternative behaviours that can reduce or eliminate the need for a restrictive practice.
PROACT-SCIPr-UK®
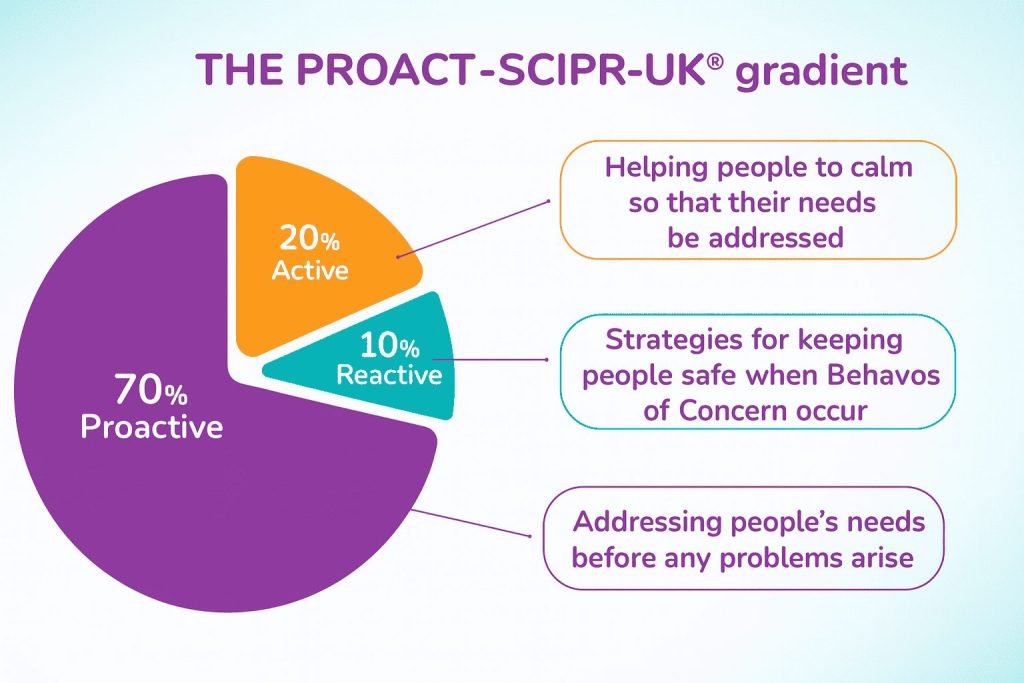
PROACT-SCIPr-UK® is a proactive approach created to reduce the use of restraint by addressing distress before it escalates. It’s rooted in understanding how people feel, what they need in the moment, and how their environment can be shaped to give them a greater sense of safety and control. Instead of waiting for a crisis, teams use early cues, structured support, and clear communication to stabilise situations and prevent harm.
This approach shifts the focus from reacting to behaviours to truly supporting the person – preserving dignity, protecting rights, and building trust. When applied well, restraint becomes the absolute last resort, not a default response, and people experience care that is calm, respectful, and centred on their needs.
Practical examples:
- For example, if someone begins pacing or withdrawing when overwhelmed, staff might offer a quiet space, reduce sensory stimuli, or use calm, familiar language to ease anxiety – preventing escalation before it happens.
- If a person shows signs of frustration during transitions, the team may use visual prompts, predictable routines, or a trusted staff member to guide them through the change smoothly.
- In moments of rising tension, rather than reacting to the behaviour itself, teams apply tailored strategies built on each person’s communication style and emotional triggers.
This way, restrictive interventions become unnecessary in most situations. PROACT-SCIPr-UK® keeps the focus on the person, preserves dignity, and builds trust, ensuring restraint is truly a last resort rather than a standard response.
Find out more in our PROACT-SCIPr-UK® brochure – now available to download for free.
Trauma-Informed Care
Trauma-informed care recognises that past experiences of trauma can shape how people respond to stress, change, and perceived threats, often influencing behaviours that may otherwise be misunderstood. By understanding the impact of trauma, carers shift their focus from control to emotional safety and trust.
In practice, this involves:
- Creating predictable, calm environments that reduce uncertainty and anxiety.
- Identifying and responding to personal triggers early, before distress escalates.
- Using compassionate, non-judgemental communication that validates a person’s feelings.
- Supporting choice and control wherever possible to rebuild a sense of safety.
- Focusing on relationships and consistency to establish trust over time.
When people feel emotionally safe and understood, distress is less likely to develop into behaviours that require restrictive interventions. Trauma-informed care doesn’t just reduce restraint — it transforms the culture of care to prioritise dignity, safety, and healing.
Person-Centred Approach
A person-centred approach is a type of approach where the person is supported to lead the way to care and recovery. The focus is solely on the person and what that person can do, not on their disability or challenges. The support provided is focused on achieving people’s aspirations so it can be tailored to their specific needs and unique abilities.
Person-centred approaches are used to ensure that the focus is placed on what matters to the people receiving support and their families. It also ensures that people are always seen as unique individuals with unique talents, contributions and gifts. The approach is a toolbox to help people while enabling them to choose their path to a positive outcome. This approach’s core principle is always to ensure that people are always listened to and kept at the core of the decision-making process.
Outcome-Based Approach
An outcome-based approach is one of the fundamental approaches in health and social care as it supports people to live their best lives by valuing their needs and building upon their strengths. Once people feel supported and listened to, they are more likely to improve their well-being and physical and mental health.
Supporting people through an outcome-based approach and developing person-centred plans makes them much more likely to succeed. The positive outcome results from progress and hard work in care delivery. It is all about making real improvements in the quality of life.
Principles of Reducing Restrictive Practices
Human rights are the foundation of people’s freedom and belong to everyone. They are based on core principles like equality, respect, dignity and independence. Human rights protect the freedom of people to control their life and take part in all decision-making processes that impact their right to receive equal services.
Providing a safe environment for everyone alongside human rights is another fundamental principle of reducing restrictive practices. It ensures that people are treated with respect and dignity. Also, a safe environment includes a space where behaviours that challenge are managed in ways that show humanity and respect. At the same time, restrictive interventions are used as compassionately as possible as a last resort when all other options have been considered.
Respect and Dignity
Dignity is a fundamental human right and a long-established principle in healthcare. Policies, procedures and rules ensure that people’s dignity is maintained and respected while receiving care.
Healthcare providers ensure that they provide care in a way that ensures people are well respected and their dignity is protected. This includes allowing for privacy when people need and want it, treating everyone equally, and providing the support they might need to become as independent and involved in the local community as possible.

Providing a Safe Environment
Providing and maintaining a safe environment reflects care and compassion for people’s welfare and is as vital as any other aspect of healthcare.
The goal of providing a safe environment is to prevent and reduce risks or harm that can occur to people during the provision of care. The basis of the discipline is to allow for continuous improvement by learning from past experiences. A safe environment is crucial in delivering effective, high-quality services focusing on people’s strengths, needs and wishes.
Recovery-Oriented Practice
Recovery-oriented practice is a massive element in ongoing healthcare reforms that spotlight the personal journey of people living with a disability.
The principles of a recovery-oriented approach include getting to know each person and learning that everyone is different and should be supported to make their own choices. This approach puts people first and understands that each individual knows best about their own life and what are the best ways to assist them in achieving their goals and aspirations.
Recovery means different things to different people. For some, it means getting support in controlling their own life; for others is acknowledging individual differences and accepting these differences. Also, focusing on recovery means that each person’s journey will unlikely be a straight path but will include setbacks and significant achievements. Being optimistic and working towards an end goal helps people with disabilities live a life based on their choices, abilities and strengths.
Respect for Individual Rights
Human rights set a framework of clear principles for respecting people’s wishes, needs, choices and differences. In healthcare, a human rights-based approach includes evaluating care policies and targeting discriminatory practices that lead to unequal outcomes.
By respecting people’s human rights, strategies and methods are designed to improve people’s lives and their rights to choose how they want to receive care.
Restrictive Interventions as a Last Resort
Restrictive practices should only be used as a last resort to prevent further harm to the individual or others. These practices should only be used when there is an immediate risk of harm for a person displaying behaviours that challenge. Still, there has to be an opportunity to de-escalate first.
Providing reassurance and allowing individuals with behaviours that challenge space and time before imposing a restrictive practice should always be considered a first port of call before applying any restrictive intervention.
Nurseline Community Services Is Dedicated to Preventing Unnecessary Hospital Admissions and Restrictive Practices
Nurseline Community Services aims to reduce unnecessary hospital admissions and focus on providing care to people in their own homes.
With our person-centred and humanised approach, we focus on what people can do. We have expert teams for crisis management and de-escalating crises, which entail a fast response to every person we support.
Our team’s compassion and continuity of care rooted in positive behaviour support practices are the core recovery principles for the people we serve. Through partnerships and collaboration, we learn about people’s needs and develop care plans based on our assessments.
Our Community Transitional Services are designed to support people as they move from hospital or acute care settings back to their home environments. This service bridges the gap, offering consistent and compassionate care tailored to each person’s needs. Our team works closely with each person, their families, and healthcare providers to ensure a smooth transition. We provide practical support, emotional reassurance, and a detailed, person-centred care plan that focuses on long-term well-being and stability in the community. Through our transitional care approach, we help people build confidence and independence as they settle into their own homes.
Discover our impact on the following link.
If you want to know more about how we can help, contact us today!